This paper studied the effect of a ketogenic diet composed largely of saturated fat compared to one composed largely of unsaturated fat. Ketogenic diets are high in fat and low in carbohydrate and protein. Ketogenic diets are known to stimulate physiological insulin resistance that goes away after a few days of eating a carbohydrate rich diet. Fat doesn’t cause much insulin to be released and I think the assumption was that if you weren’t eating carbohydrate, your body became insulin resistant because there just wasn’t a lot of insulin going around. The idea was “Well, it’s winter now, all there is left to eat are animals, so let’s just not even bother with insulin.”
It turns out that is not the case. Ketogenic diets cause physiological insulin resistance not due to lack of insulin but because of the saturated fat content.

In this chart the grey bars are people on the high polyunsaturated fat keto diet – most of the fat was from soybean oil – and the white bars are people on a high saturated fat keto diet, with much of the fat coming from meat. This chart shows that even on a ketogenic diet, with 70% of calories coming from fat, the participants who consumed most of their fat calories as polyunsaturated fat, meaning vegetable oil, remained insulin sensitive. Only the dieters eating saturated fat achieved a state of physiological insulin resistance.
So in humans, saturated fat consumption leads to physiological insulin resistance and vegetable oil consumption does not. ROS is the signal. But why doesn’t vegetable oil lead to physiological insulin resistance?
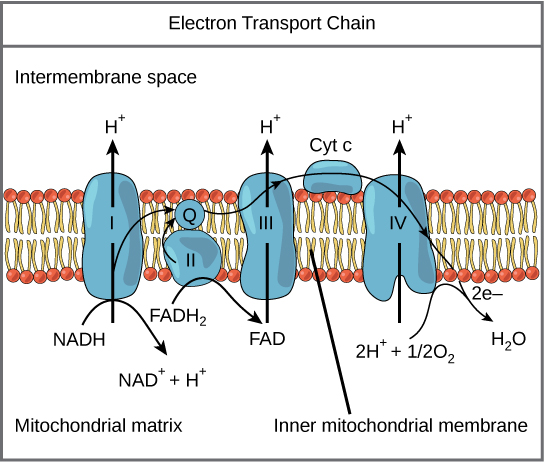
We’ve already seen that saturated fat causes physiological insulin resistance because when it is oxidized it produces a lot of FADH2, which sends a lot of electrons into the Coenzyme Q bottleneck, many of which ping back out as superoxide. Superoxide gets converted to hydrogen peroxide which then shuts down insulin signalling, leading to physiological insulin resistance.
Every time a saturated fat bond is replaced with an unsaturated bond, less FADH2 is produced, which means that less electrons are sent into the Coenzyme Q bottleneck, which means that less electrons ping back out of the mitochondrial electron transport chain which means less superoxide which means less hydrogen peroxide which means more insulin signalling.
By CNX OpenStax – http://cnx.org/contents/GFy_h8cu@10.53:rZudN6XP@2/Introduction, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=49924807
Mitochondrially produced ROS (superoxide and hydrogen peroxide) are a signal to the organism that fat is being oxidized rather than carbohydrate. This has been conserved in evolution for perhaps a billion years, as we saw with C elegans worms. The signal to the body that fat is being oxidized is the production of ROS. ROS is the signal. Unsaturated fat eliminates the signal.
