While recording a podcast with Ben Greenfield, I was discussing how the French, Tibetan yak herders and early American farmers all had a diet combining saturated fat (butter) with starch yet appeared to stay lean and healthy. Ben then suggested that there were studies showing that combining saturated fat with starch increases LPS. LPS is a bacterial toxin that can get into your bloodstream during digestion. It is generally seen as being “bad” as it can lead to inflammation1 and is typically higher in those who are diabetic.2
The answer that I gave Ben was that based on my knowledge of traditional cuisines, that doesn’t sound right but I don’t really know enough about LPS to refute it.
After the show I quickly discovered that a long term (12 week) dietary intervention trial had been conducted to determine whether or not this was true!3
Burying The Lead
Researchers randomized 75 subjects into four groups. One group (HSFA) ate a “high fat” diet (40% of calories), mostly from butter. Another group (HMUFA) ate the same amount of fat as olive oil. A third group (LFHCC – the carbohydrates were complex, they can be so complicated. The “complex” carb used was white bread and it was the same in all three groups) only ate 28% of calories as fat using both butter and olive oil. The last group (LFHCC n-3) ate the same as the third but supplemented with fish oil.
The four groups ate these diets for 12 weeks then were tested for fasting LPS. They ate a test meal that reflected the test diet they’d been eating.
Maybe Ben was right! Right there in the abstract it says:
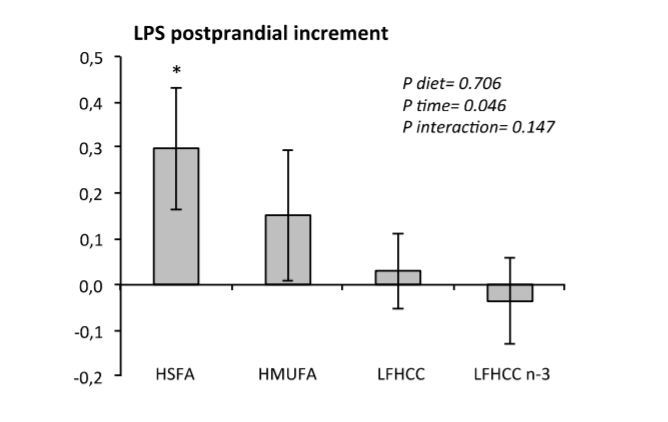
They present this graph as proof. Clearly the butter group increased post-prandial LPS the most, although I’d argue the olive oil rise looks significant as well.
But what were the fasting values for the groups after 12 weeks on the test diets?
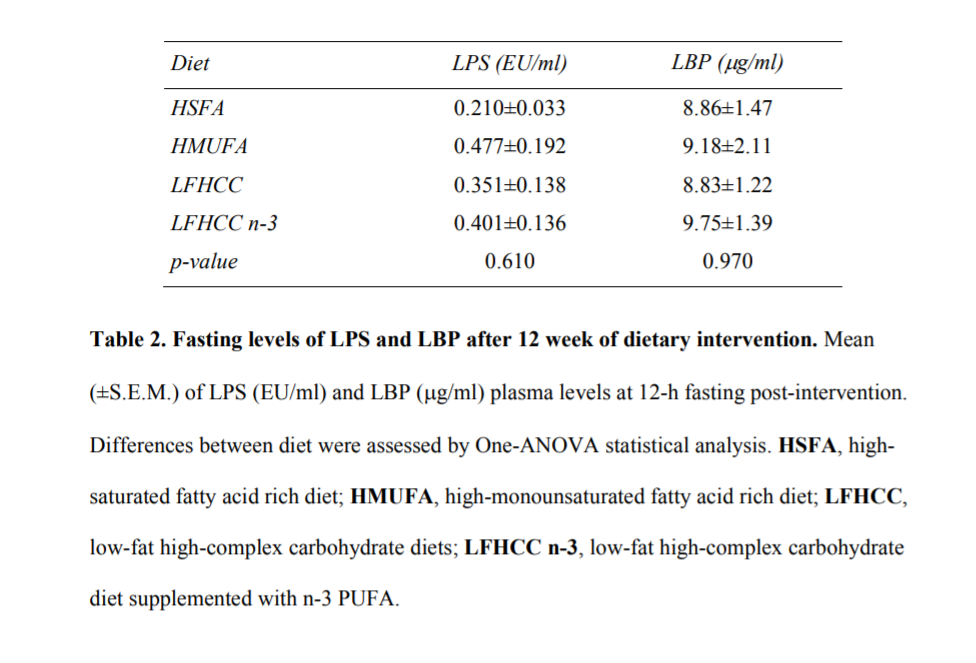
The high fat butter group has HALF the fasting LPS of the other groups. Even if there is a brief post-prandial spike, the butter group has by far the lowest overall exposure to LPS. Kind of a curious thing to leave out of the discussion, don’t you think? They ran some statistical analysis that is never explained, came up with a high p-value and therefore concluded that all of the groups are the same.
If you add the incremental post-prandial increase from the previous graph to this table of fasting values, you can see that after the meal – when butter is supposedly having it’s pro-inflammatory effect – LPS in the butter group would be 0.5, while the olive oil group would’ve been at 0.67. They never present total values, though, only baseline and the amount of change. It almost seems like they don’t want us to notice.
The only way their conclusions could be justified is if there was some massive error in the randomization of the groups. If the ~19 people in the butter group all just happen by random chance to have started out dramatically lower than the other groups. This is unlikely in a group of that size, but of course a standard study design would have been to randomize the LPS levels of the groups before the dietary trial. Yet they don’t report doing that and they don’t report the pre-diet intervention LPS levels of the groups. This is a curious omission. Overall, the study seems well done, but they didn’t randomize the groups as to the very thing they were studying? Either they are not very good or they don’t want to tell us.
Conclusions
You have to read the whole paper and not just the abstract!
I’m still no expert on LPS, but after reading this paper, I am going to stand my ground that the traditional French/American/Tibetan diet of starch and butter is probably healthful in regards to LPS exposure until proven otherwise.
- 1.Cani PD, Amar J, Iglesias MA, et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes. Published online April 24, 2007:1761-1772. doi:10.2337/db06-1491
- 2.Pussinen PJ, Havulinna AS, Lehto M, Sundvall J, Salomaa V. Endotoxemia Is Associated With an Increased Risk of Incident Diabetes. Diabetes Care. Published online January 26, 2011:392-397. doi:10.2337/dc10-1676
- 3.López-Moreno J, García-Carpintero S, Jimenez-Lucena R, et al. Effect of Dietary Lipids on Endotoxemia Influences Postprandial Inflammatory Response. J Agric Food Chem. Published online August 22, 2017:7756-7763. doi:10.1021/acs.jafc.7b01909

That’s interesting, Brad. You should run this by Gabor Erdosi.
Sorry this is ot but what about bee’s wax? Is it high in stearic acid? Apparently it’s edible and it could be categorised as an animal food for the carnivore crowd. It’s pretty hard at room temp. Hmmm
Honestly, this is the first time I’ve thought about it. I have no idea what bee’s wax is made out of.
I’m sure leaving that important information obscured is just a coincidence…
Thank you Brad, nice digging!
I am contemplating this diet, for one my hubby is sold already! He told me there is such a thing as “a drinking man diet” – have you heard of that? It sounds very close to yours! By the way the author of that diet lived till 98!
On a side, coming from keto world, can I just double check with you, that we need carbs on this protocol for the reason of “confusing” the mitochondria, who get 2 streams of electrons coming in, from carbs and from fat, pushing electrons into reverse cycle ie rendering cells insulin resistant? And carbs ARE essential for that? Cheers!
Hi! I don’t think the carbs are essential. Carbs and fat shouldn’t be oxidized in the same cell at the same time due to something called the randle cycle. So any given cell should be burning one or the other.
Carbs ARE great as a vessel for fat and I think the post-prandial rise in BG from starch helps my satiation, although some disagree with this.
What about people with APOE4? You know, the gene that must keep saturated fats to a minimum?
Would love it if you could write a post about this.
I haven’t had the opportunity to research this but it’s on my topics of interest list.
Rather than making butter + stearic in oil form, any thoughts about whipping the stearic acid powder into soft butter using a KitchenAid mixer? Hystrene Stearic Acid is such a fine powder that it can be whipped into butter and it remains suspended. I am just not sure about the bioavailabilty of the Stearic Acid in this form and if it could cause gastro-intestinal distress, but I believe the texture and flavor would be closer to real butter.
This is a common question: is the powder absorbable on its own? The answer is I don’t know. Some people seem to have gotten results this way, my guess is that it’s significantly less absorbable in powdered form. I don’t know how much less.
Is your butteroil back in stock? I would love to try it.
Thx,
Chris
It’s back in stock as of today!
Hello Brad. I heard your podcast with Paul Saladino, and have actually gone back and re-listened twice.
Excellent information! I would like to try some of the butteroil as soon as it’s available. I subscribed to email list. Will someone contact me when butteroil ready to ship?
Thank you,
Chris
The newsletter should go out TODAY announcing that butteroil is back on sale.
Hi Brad, I understand the stearic acid component, but why starch per se? Could we just as well pair these fats with other carb sources such as fruits, dried fruits, pure sugar, etc? Is it just that starch provides a natural assimilator or conduit for these fat sources or is there a biochemical action behind these specific carb sources?
I suppose you could use others carbs… I like starch because it’s traditional – croissants, pancakes, french fries, etc. It’s also VERY fat absorbent. The only downside I could see to using fruits is that sugar upregulates SCD1, which unsaturates the stearic acid and works against you. Then again so does insulin, which is maximally produced by combining starch with saturated fat. So it might be a wash.
Cannot buy from your web shop. I am in Europe. It just fails completely. Love your blog. Let us know when / if anything is available.
Odd, I do sales to Europe all of the time. There is sometimes a browser specific issue, try a different device or browser.
Hi Brad great stuff…How to make the Butter oil from butter and steric acid?
The easiest way is just to melt butter and then add stearic acid little by little until it gets waxy in your mouth. If it gets too waxy add back more butter and/or MCT oil.
Hi Brad! This is not related to the topic of this post, but I am wondering whether you would be interested to have a discussion with Bart Kay. He thinks that it is not a good idea to combine carbs with fats, and that this would inevitably make you fat. Since your experience is quite to the contrary, I am sure you both would have an interesting discussion:-)
Sure, I’d love to! There are many others in the keto community who believe that combining starch and fat always leads to obesity. But then, how do you explain France before they started eating sunflower oil?
I try to click on the link to buy your bacon, but it is a loop that only goes back to the home page. How does one sign up for the bacon?
Hi! Firebrand Meats website was screwed up for a couple of days as I migrated servers. It’s back now.
Sounds like you’re in the process of rediscovering what Ray Peat figured out decades ago. “The Bio-energetic Theory of Nutrition”. Lets see you two do a podcast together!
There is a lot of crossover with Ray Peat, but I haven’t had the time to read up on his work.
Is stearic acid causing insulin resistance in other than adipocytes cell types as well?
In general, studies have shown that it tends to lower BG as I recall. I don’t know why, exactly. Of course it could be causing other tissues to become IR, I suspect there hasn’t been a lot of science done on it.
I have now officially read every article on this site… so fascinating!
I just had an “ah-hah” moment in the bathtub… what if PUFAS are altering not just how our fat cells work, but are alteting the function of other cells that utilize lipids… specifically skin cells? Our skin has a lipid layer that is supposed to provide protection from the outside world. If our lipid layer is made of PUFAS, and PUFAS oxidize when exposed to heat and light, could sunlight be oxidizing our PUFA-made lipid layer, contributing to (or maybe directly causing) skin cancer? Just throwing it out there, I think its an interesting thought…
I 100% agree with your AHA moment and have believed that for a long time.