In my last post I recommended a strategy of combining lipoic acid – a natural, mitochondrially produced substance which oxidizes NADH to NAD+ – and succinate, which drives mitochondrial ROS production and oxidation of NADH to NAD+ via the activity of the enzyme NNT. Both of these are designed to shift the redox pool of NADH to a more oxidized state as defined by a high NAD+/NADH ratio. High levels of mitochondrial NAD+ should activate SIRT3, leading to the deacetylation of our mitochondrial enzymes. NAD+ is also a required co-factor in the citric acid cycle. The more mitochondrial NAD+ you can regenerate, the faster you can run your metabolism.
Since that post I’ve been lurking over at the Reddit r/SaturatedFat to hear people’s experiences. One of the things people have been reporting are symptoms resembling the so-called “keto flu” – headaches, lethargy and sometimes even nausea. With most these symptoms seem to subside within a few days as they adapt. Someone suggested that perhaps the symptoms were due to dropping blood glucose level, although no one was reporting a rapid drop in blood glucose due to either supplement. I suspect the symptoms could be due to rapidly dropping lactate levels.
In theory, succinate and lipoic acid should have the same effect on NADH/NAD+ ratios and lactate levels, but a lot more is known about the effects of lipoic acid than succinate, so I’ll focus there. I also like the alliteration.
Lactate as a Circulating Redox Buffer
The traditional view of metabolism is that glucose enters a cell, is broken into two molecules of pyruvate via glycolysis and the two pyruvate molecules are shuttled into the mitochondria to be fully oxidized. This recent review1 presents an alternative viewpoint. In most cells glycolysis and mitochondrial respiration are uncoupled. Monocarboxylate transporters (MCTs) are rapidly excreting and re-uptaking lactate and pyruvate.
In the cytoplasm, lactate dehydrogenase catalyzes the reversible reaction of converting lactate to pyruvate while reducing NAD+ to NADH. This reaction is controlled by the relative ratios of NAD+/NADH and lactate/pyruvate. A cell with a high cytoplasmic NADH/NAD+ ratio imports pyruvate, reduces it to lactate – converting an NADH to an NAD+ – then exports it, thus lowering it’s NADH/NAD+ ratio.
The authors suggest that glucose serves as a fuel for specific tissue types that require it but that lactate is the true universal carbohydrate fuel.
in mammals, lactate also serves as a major circulating carbohydrate fuel. By providing mammalian cells with both a convenient source and sink for three-carbon compounds, circulating lactate enables the uncoupling of carbohydrate-driven mitochondrial energy generation from glycolysis. Lactate and pyruvate together serve as a circulating redox buffer that equilibrates the NADH/NAD ratio across cells and tissues. This reconceptualization of lactate as a fuel—analogous to how Hans Christian Andersen’s ugly duckling is actually a beautiful swan—has the potential to reshape the field of energy metabolism.
Joshua D. Rabinowitz and Sven Enerbäck. “Lactate: the ugly duckling of energy metabolism”
The authors go on to suggest that overall levels of lactate are largely affected by the activity level of pyruvate dehydrogenase (PDH) – the mitochondrial enzyme that converts pyruvate to acetyl-CoA, initiating mitochondrial respiration. To say this simply, when pyruvate is oxidized in the citric acid cycle, circulating levels of lactate drop. PDH controls the rate at which pyruvate can be oxidized.
I previously wrote that PDH activity is low in both torpid animals and obese humans due to its inhibition by PDK4, which phosphorylates it and turns it off. In turn, PDK4 is activated by NADH and Acetyl-CoA.2 In obesity, buildup of mitochondrial NADH leads to fewer turns of the citric acid cycle, which allows acetyl-CoA to build up. The acetyl-CoA and NADH activate PDK4 which phosphorylates PDH and turns it off.
Lactate In Obesity and Diabetes
Fasting lactate and pyruvate levels are increased in obese and obese diabetic humans:3
| Lean | Obese | Obese Diabetic | |
| Blood Lactate (mmol/l) | 1.78 | 2.26 | 2.76 |
| Blood Pyruvate (mmol/l) | 0.06 | 0.09 | 0.13 |
| Blood Glucose (mmol/l) | 4.5 | 4.8 | 11.7 |
Lipoic Acid Reduces Circulating Lactate
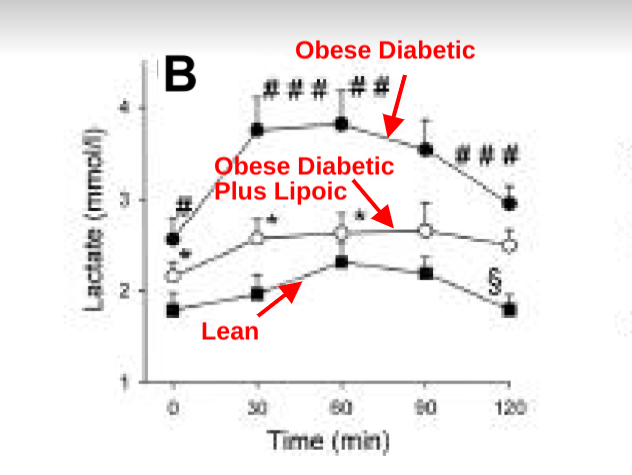
Obese, diabetic patients who took 1200mg (600mg twice a day) of lipoic acid for 4 weeks saw a significant drop in circulating lactate both in the fasted state and in response to an oral glucose tolerance test.
R-Lipoic acid allows the direct oxidation of mitochondrial NADH to NAD+. NAD+ allows the citric acid cycle to cycle, reducing acetyl-CoA. Lowered NADH and acetyl-CoA increase PDH activity. Increased PDH activity allows more lactate to be fully oxidized (as pyruvate). When lactate is being burned in any tissues, systemic lactate and pyruvate levels drop due to the rapid flux in and out of cells.
Lactate, Nausea and Headaches
According to Wikipedia, Ringer’s lactate solution (RL), also known as sodium lactate solution and Hartmann’s solution, is a mixture of sodium chloride, sodium lactate, potassium chloride and calcium chloride in water. It has been in use since 1930 and is on the Wold Health Organization’s list of essential medicines. Ringer’s lactate is the standard of care for preventing post-operative nausea.4 It is also sometimes used for headaches.5
An n=1
All of this gives me an idea for an n=1 to wedge between Thanksgiving and Christmas. I bought a blood lactate tester over a year ago and have barely used it. I’ve been going through a washout period (no supplements) to establish a baseline to do a better n=1 with lipoic acid and Succinade. I’m going to collect baseline levels of lactate throughout the day for three days, followed by escalating lipoic acid. When I’ve hit 2400mg, I will plateau and escalate Succinade. I’m still thinking through details, but I like the idea of lactate as an indicator of PDH activity.
Conclusions
I suspect that a rapid drop in lactate levels could causes symptoms such as headache, nausea and lethargy. I also suspect that dropping lactate levels are an indirect indicator of increased pyruvate dehydrogenase levels: moving away from torpor. We know that lipoic acid drops lactate levels in the medium term, but I’m going to see how it behaves in the short term – minutes to hours – and if succinate will have a similar effect on lactate.
- 1.Rabinowitz JD, Enerbäck S. Lactate: the ugly duckling of energy metabolism. Nat Metab. Published online July 2020:566-571. doi:10.1038/s42255-020-0243-4
- 2.Pettit FH, Pelley JW, Reed LJ. Regulation of pyruvate dehydrogenase kinase and phosphatase by acetyl-CoA/CoA and NADH/NAD ratios. Biochemical and Biophysical Research Communications. Published online July 1975:575-582. doi:10.1016/s0006-291x(75)80185-9
- 3.Konrad T, Vicini P, Kusterer K, et al. alpha-Lipoic acid treatment decreases serum lactate and pyruvate concentrations and improves glucose effectiveness in lean and obese patients with type 2 diabetes. Diabetes Care. Published online February 1, 1999:280-287. doi:10.2337/diacare.22.2.280
- 4.Salman N, Aykut A, Sabuncu Ü, Şaylan A, Yağar S, Şekerci S. Dextrose administration may reduce the incidence of postoperative nausea and vomiting after laparoscopic cholecystectomy: a double blind randomized controlled trial. Minerva Anestesiol. Published online April 2020. doi:10.23736/S0375-9393.20.13484-9
- 5.Carter BL, Pasupuleti R. Use of Intravenous Cosyntropin in the Treatment of Postdural Puncture Headache. Anesthesiology. Published online January 1, 2000:272-272. doi:10.1097/00000542-200001000-00043

Hmm…my mind first went to metformin (and maybe berberine?), which apparently increases circulating lactate. How does that fit into the story? The paper above (ref 3) says that the patients who were taking metformin were taken off it a couple of weeks before this study. I wonder, if taken together, this effect would be cancelled out – although I don’t know the relative magnitudes of the effect. Does metformin increase lactic acid to the same extent as LA decreases it?
The other thought I had was again about NR or NMN supplementation. I know you wondered whether increasing the pool size of NAD+ might not make a difference on its own… but I do wonder if it might…. as you say “NAD+ allows the citric acid cycle to cycle, reducing acetyl-CoA.”
I’m not deep into the biochemistry though as some of the other commenters here and on reddit are, so this is some high level hand waving here.
Thank you for asking this. I’m very interested as well, as I take Metformin and was considering adding R-ALA to my regimen.
Jenn
Yeah, I’ve also wondered if the effects of berberine/metformin might limit the usefulness of this approach, since you can’t drive ROS if complexI is partially blocked. Probably worth doing a post on…
Hi Brad,
So where would Astaxanthin come in on all of this??? Should we avoid using this also???
Does Metformin/Berberine block Complex I? I might have either missed something previously, or misunderstood you just now.
Anyway I just ordered some ALA and will begin taking it tomorrow. Still taking Metformin (1000mg every evening).
Yes, berberine and metformin are both mild inhibitors of complex 1, causing an artificial “energy shortage” which increased AMP which activates AMPK. All of which can be useful, although in an ideal scenario you would have full electron flow through both complex I and II. I’m wavering on berberine/metformin.
Brad
Added:
A quick Google search sort of made my previous question dumb. LOL
I take Metformin for SCD1 inhibition (you had mentioned it was a powerful inhibitor waaaay back in the beginning) but I’m not necessarily attached to it beyond that.
I also take G. pentaphyllum and Hesperidin, so maybe those are sufficient and I can shelf the Metformin for a while.
Or keep taking it at first…
Honestly, whichever is more beneficial to our ongoing research. Just let me know. 🙂
Jenn, I stopped taking Berberine as I started on R-ALA; in fact I stopped everything else except vitamin D and Magnesium. It has only been three days. I am happy I stopped the Berberine as I do have some side effects from the ALA and don’t want to overload my body (though, I see that in Europe diabetics often take metformin and ALA together).
The day I first took the higher dose of R-ALA (600mg) I have had a headache all day (manageable with paracetamol, but had to take it twice during the day), a spaced out sort of feeling and a funny feeling in my stomach (? precursor to heartburn/reflux). I don’t feel nausea, but my appetite and interest in carbs has been much much lower than usual today (day 3). My overnight fast is usually around 12-13 hours, but today it was 17 hours pretty effortlessly…. I just didn’t feel like eating. So far the side effects are manageable. I am going to have a big meal after the ALA today to see if that helps the heartburn.
So far so good and I feel optimistic about this.
Thanks Meg!
I started yesterday with 1200mg of mixed R-ALA and ALA. and ditched my Metformin dosage yesterday. I’m not sensitive to supplements at all, so I just jumped right in. Brad said ALA seems generally well absorbed so I figured I’d get what was readily available and affordable at high dosage and went with a mix.
I did have a bit of a headache but didn’t even need medication. I have a weird “spacey feeling” sometime about 20-30 mins after taking the ALA but it passes in about 5-10 min.
My blood glucose was FANTASTIC on the ALA yesterday, but I had a bit of a sugar binge (very very unusual for me, not related to the supplement, just coincided with starting it) so my recorded stats are less relevant than they will be in the coming days.
I’m going to track my stats daily similar to how Sandra did in her story. I’m not taking succinate, but honestly, I’m not sure it’s the “magic bullet” anyway as much as the ALA is. We’re producing succinate as we burn carbs and fat – even if we’re fasting and it’s body fat. Less so, perhaps, if we’re highly unsaturated.
I should say that diet-wise I’m not exactly doing TCD. My attempt at TCD was… Unsuccessful. LOL My hubby did better and he actually still eats according to the principles now, although his losses are very slow unless he manages his carbs a bit.
I mostly eat lean protein when I do eat at all, so I’d say I’m generally completely fasted and only eat some bites of lean protein to satiety 1-2x a day. I’m comfortable and happy all day. I’m very low calorie because of the nature of the foods, but not hungry at all. I will let my body’s hunger dictate if my diet needs to change as I approach goal, but right now I actually think it’s happy to be able to offload some of my stored energy and the thought of eating often repulses me when I’m deep into ketosis.
I can’t lose weight on anything but lean protein. It’s just not possible for me. I think I must have been desaturating my dietary and body fat constantly before which is why lean protein (which takes out the fat factor entirely) is all that has ever worked for me in my life. Even keto didn’t work very well because my SCD1 was presumably overexpressed and I was packing all my fat away as MUFA.
Funnily, next to lean protein (which consistently works extremely well for me) I’ve had the best luck in the past with high MUFA, low Sat Fat Mediterranean. I wouldn’t say it was great for LOSS, but I was maintaining well for MONTHS eating all the pasta and bread I could ever handle, dipped in olive oil and topped with cheeses. I was essentially vegetarian bordering pescatarian during that time. After reading Brad’s research I think it’s because the MUFA was triggering satiety while the heavy amounts of starch were substrate for my body to generate Sat Fat. I also ate a LOT of cheese (CLA) which was probably helping to suppress SCD1 a bit. Anyway, I wouldn’t go back to this way of eating again but it is fascinating to me that it’s the most success I’ve ever had at maintaining and it really lines up with these principles here. 🙂
Anyway…
Other supplements I continue to take are:
Gymnostemma
Hesperidin
Salted Natural Calm (Magnesium drink)
I occasionally take a few pink salt rocks if I’m feeling electrolyte depleted but not hungry.
Pu-erh Tea MOST days, several cups. Not every day but probably 4-5 days of the week.
I figure I want to keep suppressing SCD1 while I lose weight, hence keeping my supplements.
I’m feeling optimistic too, and I’m excited to see how my stats change over the coming 30 days. The reading I’ve been doing seem to suggest we’ll see good results from the ALA alone and that the additional succinate might not be necessary at all or even optimal for everyone. I do think I’ll order some Succinade and experiment with that in the future if I have trouble getting out of torpor just by burning off my body fat.
Thanks for the detailed posts. Dietary MUFA has some distinct differences from SCD1 generated MUFA. In addition to the OEA, olive oil actually contains some very interesting polyphenols that have shown to be of benefit. MUFA is still not my favorite, but your experience is interesting.
Brad
Interesting … I’ve always thought of lactate as a negative thing so this is definitely a new perspective.
Lactate, hmmm… I was born allergic to all milk, almost died of starvation till the geniuses around me figured it out and put me on soy, what IS lactate? is it like lactic acid when you exercise too much? or is it like lactose as in lactose intolerant .. sorry, i just woke up, it’s probably neither, seems a natural byproduct of things, but i just wondered why they call nursing mothers ‘lactating’, maybe i have a sort of vestigial tail of childhood allergy left? and if i did, would it matter? ok, need coffee… thanks for this, Brad!!
It’s the lactic acid when you exercise. Not much related to lactose in milk IIRC.
Hi Elaine! It’s a good question, actually! Lactose is a sugar found in milk. Lactate is a fermentation product, that was initially found in cheese or some fermented dairy product, hence the similar name. But we all have circulating lactate and yes it is what builds up in exercise.
I also got headaches with Hesperidin. Do you think that is along the same lines?
IDK, really.
I’ve been taking 1,200 mg lipoic acid in the morning with my coffee, then one scoop of succinate prior to my first meal (lunch). The things I’ve noticed:
– The lipoic acid upsets my stomach/makes me hungrier.
– The succinate has to be taken with a lot of water, else I get sick to my stomach.
– It’s hard to remember to take succinate an hour before eating, just based on my particular schedule.
– Effects are unclear. Temperature is ambivalent. If temp does increase, it takes hours. For instance, I took succinate around 10am; just took my temp and it was: 96.3 at 9:18am (got into work); 96.8 at 12:26pm; 97.8 at 2:09pm.
– I did not take my temp before starting the regimen, so it could be this is normal for me. I made the mistake of not getting a good baseline.
– I did take 1/2 scoops morning and night for one day, but got hot at night and had poor sleep. Decided only one scoop during the day for this week. Not sure if the poor sleep was succinate-related or random.
– Seems to cause hard defecation for me. Unusual.
I’m still testing. Will add in a 1/2 scoop in the evening at some point.
Oh yeah, did have to take an allergy pill and an advil the other night, which never happens. I can’t remember the last time I took either one; last year sometime, I think.
After reading that Reddit thread, I guess I should have been taking my temperature in the morning instead. I’ll have to try that.
I remember reading about the idea of lactate as part-processed carbs (here?) and liking it. Seems analogous to ketones being part-processed fats. Between the two of them, they create a flexible way of starting the burning of fat or glucose in a place in the body that has plenty, then moving the intermediate (lactate / ketones) to a different part of the body (optional), then finishing the burning. Seems very neat.
That is correct, but what’s even cooler is that cells can equilibrate their NADH/NAD+ ratios by taking in pyruvate and releasing lactate (which converts NADH to NAD+) or vice-versa.
Thinking out loud here… And this might be Capt. obvious/oblivious.
Given that muscle exertion produces lactate. Could the lactate be doing a few things here?
1. Saturating the cell with the primary particle it needs to be able to ramp up processing of any energy (fat/glucose) that it can get it’s hands on. My minds eye sees the cell as a drowning person that’s gasping for air but can’t get any and flailing arms trying to grab onto anything to stay afloat.
2. Pain as a rate limiter to prevent cellular damage while it waits on the energy processes to catch up. Only so much blood volume can pass by within a given time frame. Just like a car engine, if you start building it to make more and more power, but don’t provide enough fuel and the air/fuel ratio gets lean, the processes start breaking down and very bad things happen. The pain is a deterrent to continuing that activity to prevent a “lean” air/fuel condition.
I’d love to see the insulin and triglyceride levels in that lean/obese/obese-diabetic chart since pre-diabetics (can you be obese and not be pre-diabetic/diabetic?) can have normal blood sugar levels. My guess is if the chart had these two metrics they would both be elevated as well in the obese/obese-diabetic because “insulin resistance”.
Here is the full paper by Evanna L. Mills et al. that stimulated interest in sodium succinate
Accumulation of systemic succinate controls activation of adipose tissue thermogenesis
https://www.repository.cam.ac.uk/bitstream/handle/1810/283464/Binder1.pdf?sequence=1&isAllowed=y
Thanks for the non-paywalled post. It’s a good paper.
and in their latest paper, Evanna Mills et al. works through the interaction of UCP1/BAT/ succinate/ thermogenesis and cold.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8207988/
“The newfound role for UCP1+ adipocytes as regulators of liver extracellular succinate also suggest that these cells can be leveraged to treat pathologies driven by chronic inflammation and fibrosis that depend on SUCNR1 signaling. Moreover, these discoveries provide a potential explanation for the longstanding observation that tissue extracellular succinate levels are substantial and dynamic. Tissue extracellular succinate concentrations are elevated in response to acute interventions like tissue hypoxia59, exercise60, and exposure to cold temperatures5. In the context of these acute physiological adaptations, succinate elevation is transient, and rapidly renormalizes. In contrast, in the setting of metabolic disease, circulating succinate levels are chronically elevated, a phenomenon which correlates with poor prognosis6–8. Therefore, a prediction of our findings here is that UCP1+ adipocyte content and activity will be linked to these adaptive and maladaptive processes by acting on extracellular pools of succinate. Taken together, our data therefore provide evidence for a major newfound physiological role for UCP1+ BAT and beige fat in regulation over liver extracellular succinate, independent of the historical view of these cells as regulators of whole-body energy expenditure and adiposity.”
thought experiment- if successful use of succinate depends on effective UCP1 expression , then my first approach will be cyclic- banana milk shake with 25g of stearic acid for mitochondria fusion to see if we can get improved UCP1 , then follow with slow ramping up of succinate/ALA over a week.
I love the concept.
Due to nausea ….restarting low dose alpha lipoic acid 300 mg and soon to 600 and ultimately 1200mg if I can tolerate, then succinnade 7gm in divided doses/ day and hope for the best.
Bass temps now about 97.4 to 97.7. However this not a real baseline as 1 yr of LA lowering and starting temp of more like 96.5.
Currently eating more and weight gain but slow. If I was more careful I think it would not happen.
Peak temps around 98.5
Nightly Campari/ Jägermeister neat
It’s a digestif! Dontcha know 😉
I meant 7gm/day in 3 divided doses. This stuff is kind of nasty.
Hi Brad, I’ve been following your posts with interest, I’d like your take on the paper below when you have a chance.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5581152/
Best Regards, N
Yes, I’ve seen this paper about the role of succinate in cancer. Much of the paper is about how in many cancers you see a lack of succinate dehydrogenase (SDH) activity – just like in obesity. So succinate can build up in cancer cells due to lack of SDH activity. The approach of using ALA to deactylate SDH will hopefully turn it ON, the opposite of what is being seen in cancer cells.
In some pathologies, you see a rise in circulating succinate. This is due to a global lack of SDH activity: no one can burn the succinate so they’re exporting it. The goal of ALA plus succinate is to get SDH working again and then feed it. We will know if this strategy works if our body temperature rises, our fasting blood glucose and lactate drop, etc. Furthermore, what we want to happen is to take the succinate into our cells and burn it, thus leading ultimately to LOWER circulating levels of succinate, as counter-intuitive as that might sound.
The paper also mentions the potential pro-inflammatory effect of the succinate receptor (SUCNR1). I mentioned this in my article, but there are equal numbers of papers suggesting a anti-inflammatory role for succinate, so it’s hard to really characterize this. The paper about muscle fiber type switching from glycolytic to oxidative – like in lean people – suggests that SUCNR1 plays an important role in this seemingly beneficial transition.
This leaves the question of HIF, which I don’t know enough about to comment on.
Also worth pointing out. This is a Chinese paper published in a relatively minor journal. Sometimes there are great Chinese papers. Grain of salt, though.
I had a headache for three days followed by nights of high heart rate and heavy sweating. Turns out my avg blood glucose has gone from 90-100s to 60-80s. While technically not hypoglycemic, I believe I am feeling those symptoms due to my previously higher than normal setpoint for all the associated signaling systems and regulatory subroutines.
Wow, obviously those kinds of symptoms are not what you want. On the other hand, the drop in blood glucose is certainly suggestive that something is happening.
Abdominal fat accumulation prevented by unsaturated fat
https://www.sciencedaily.com/releases/2014/02/140224110017.htm
Any idea of why they got this result, they used palm oil, maybe the problem is with palm oil and not with other sources of saturated fat, any thoughts?
Yes, the famous Muffin Study. I actually think about it all of the time, nor is it the only study showing palm oil to be more fattening than soybean oil. Here is my working theory.
If we think of lipogenesis as a self-reinforcing state of fattening that is evoultionarily conserved for the purpose of hibernation, then anything that causes circulating fats to “look like” lipogenesis should be a trigger to store fat. Lipogenesis is triggered by PUFA but the end-product is mostly palmitic and oleic acid. Stearic acid is very low during lipogensis as it is efficiently converted to oleic. Palm oil is roughly even parts palmitic and oleic acids with very little stearic and about 10% PUFA. It “looks like” lipogenesis more that perhaps any other dietary fat.
I need to get more evidence before I’d really push this in a big way.
Brad
An update. I stopped taking everything so I could take a third dose of covid vaccine. Did not want too many items to cause potential side effects. It’s been 2 weeks since the vaccine, and if there was a side effect, I don’t know what it was.
So, I’ve restarted taking lipoic acid, only 600 mg/day. I’m going to do this for 1-2 weeks (depending on side effects, if any), then up that to 1200mg/day for 1-2 weeks, again depending on side effects. Then re-start the succinate if all goes well.
I’ve started taking my temperature within a few minutes of waking, using an under-tongue thermometer:
12/4: 98.4
12/5: 98.0
12/6: 98.0
Started taking lipoic acid after the 12/6 reading. Taking “nothing” before then.
Well, those are WAY higher than I thought they would be.
As for “nothing”, I restarted eating natto again, for about a week before the first temperature reading above. I have no idea whether this has an effect, though I find those temperatures to be higher than I anticipated. Unfortunately, I never took my temperatures in the morning, only during the day at random times. Those were much lower, even in the 96.x range. But they weren’t morning readings. And pre-natto, too.
Will update again, probably in a different post by Brad, in a few weeks.
My understanding is that if your body temperature drops during the day or after eating (mine does) it’s indicative of hypothyroid. So we want to see the morning temp being the lowest and temp increasing during the day, especially after eating. I could be wrong on this and happy for correction – but all the research I’ve done suggests hypothyroid if food/time makes our temps drop. Good to know, though, and that’s what we’re working to fix right! 🙂
I remember reading that lactate may be the preferred fuel of the brain, rather than glucose. Was thinking recently that it might make sense evolutionarily since in fight or flight when your muscles are working hard you’d be producing lots of it and would also benefit most from peak brain performance in those moments.