So I do everything wrong, kind of on purpose. I eat white flour and dairy. I combine starch, protein and saturated fat. I drink black coffee and/or red wine all day long. MANY/MOST OF MY MEALS ARE DEEP FRIED.
My sleep habits are haphazard at best. This is the time of year when they are the worst. Something about the shortening days of fall gives me maximum insomnia. This year hasn’t been the worst but I’d rate my sleep as not great.
I’m doing a new dietary trial, which I think you’re going to find VERY interesting, but I’m not quite ready to talk about it so check back in on that. What I want to talk about here is my pre-trial inflammatory markers.
When I was recording my podcast with Ben Greenfield, he mentioned that combining saturated fat with starch could possibly elevate levels of LPS, a marker of intestinal permeability and, therefore, inflammation. I’ve already written about that here.
It actually caught my attention, because I also do several other things that are supposed to increase gut permeability and therefore inflammation, including – as I said – eating white flour, fried food, drinking lots of ethanol and eating dairy on top of my irregular sleep pattern. I’m also coming down from a BMI that was recently 38, showing that I probably also have or had metabolic syndrome. I’m 45 years old.
I should be a walking tower of inflammation!!!
Inflammation Vs. ROS
Inflammation and ROS are often conflated in people’s minds. They are two distinct processes that are often correlated. Inflammation is mediated by your immune system. INFLAMMATION IS AN IMMUNE PROCESS. ROS can be produced by your immune system but is also produced in the mitochondria as a signal to the cell that fat is being burned.
ROS in overwhelming quantities can be quite dangerous and the immune system uses ROS as one of the tools in its bag for fighting off invaders. For instance, phagocytes – immune cells that are crucial for fending off infections from bacteria at the site of a wound (for instance) have embedded NADPH oxidase enzymes in their membranes that can release a stream of ROS to literally burn invaders to death. This is kind of like a miniature fire tornado in your body caused by your immune system.
So your immune system uses ROS as a tool in its toolkit!
It’s less clear, but it’s also likely that ROS production can stimulate inflammation. To quote a recent paper:
And so inflammation can cause ROS production definitely and ROS production can cause inflammation, probably. But that does NOT mean that ROS equals inflammation or vice versa! They are two distinct processes that interact with each other.
My Diet
I’ve been eating a diet for most of the last 15 months designed to promote maximal ROS production in my mitochondria as a signal to the cell that I’m burning fat and therefore my metabolism should act appropriately. I believe that the consumption of polyunsaturated fats – found in vegetable oils, nuts, olive and avocado oil and in the body fat of livestock fed grains – results in a pathological lack of ROS production in the mitochondria, which in turn leads to metabolic dysregulation.
ROS is the signal.
Therefore I’ve been eating a diet very high in saturated fats that minimizes polyunsaturated anf monounsaturated fats. My preferred sources of fat are butter, stearic acid enhanced butteroil, pastured beef suet, cocoa butter and low-PUFA pork.
I consume these fats with wine, resulting in maximal mitochondrial ROS production with the goal being physiological insulin resistance in my fat cells. When my fat cells ignore insulin they release fat as energy to the rest of my body. I describe this all in the series The ROS Theory Of Obesity.
Blood Results
I just got a bunch of bloodwork done – I literally got the results yesterday – in part to answer the question of whether my diet of saturated fat combined with white flour, dairy and wine was causing inflammation. I did two separate analyses: I got my red blood cell lipid profile at OmegaQuant and I got my C Reactive Protein (CRP), Tumor Necrosis Factor-Alpha (TNF) and Interleuken-6 (IL-6) tested thanks to ownyourlabs.com, the testing service run by the always amazing Dave Feldman and Siobhan Huggins.
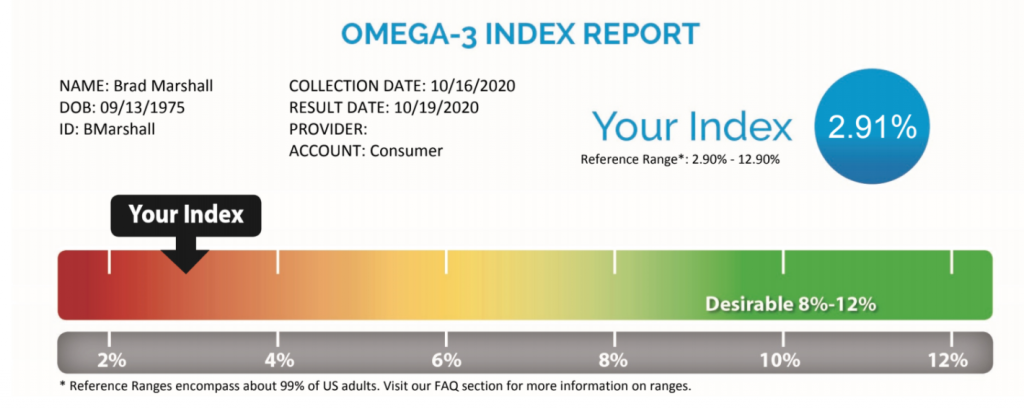
The OmegaQuant results added more fuel to the fire. My red blood cell membranes are VERY low – off the charts low – in “anti-inflammatory” Omega 3 polyunsaturated fats. The range of scores, according to them, encompasses 99% of the population. I was well outside of the range (2.4%, the low end of the range is 2.9%). My Omega 6 fats – which I’ve been purposely avoiding – were also at the very bottom of the range.
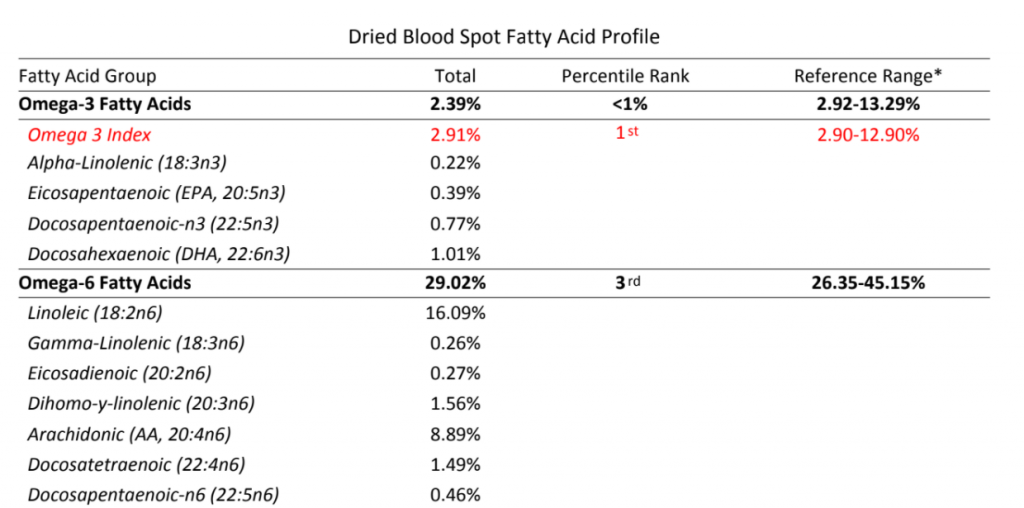
My ratio of Omega 6 to Omega 3 fats is also terrible by traditional standards. According to OmegaQuant I am “in the red”:
Now you all know my birthday. I expect a card.
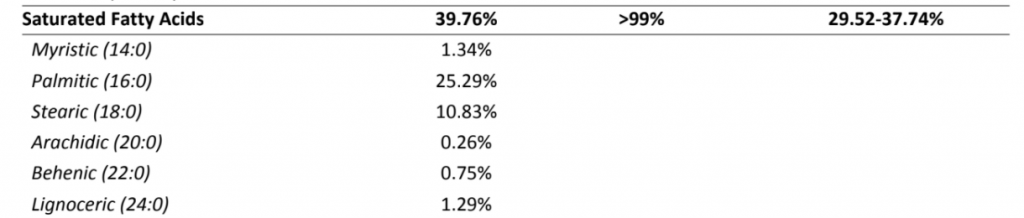
I am WINNING at saturated fat, though! I’m off the charts high!! At 39.7% saturated fat I am fully 2 percentage points higher that the highest people in 99% of the population, who check in at 37.7%.
OK. Let’s do a summary before I tell you the results:
- I eat a diet that I PURPOSEFULLY designed to generate ROS
- My Omega-6 to Omega-3 ratio is “in the red”
- I lack polyunsaturated fats in general and am high in saturated fats
- I eat tons of fried food (made at home, fried in pastured beef suet)
- I stay up late drinking wine
- I recently had a BMI of 38 with significant abdominal (visceral) fat, known to be linked with inflammation
- I eat white flour, cornstarch and dairy daily
- I drink tons of coffee
- I’m 45
- My sleep habits are bad. Even as I write this, it’s 1am.
Get to The Results Already!
OK, here they are:
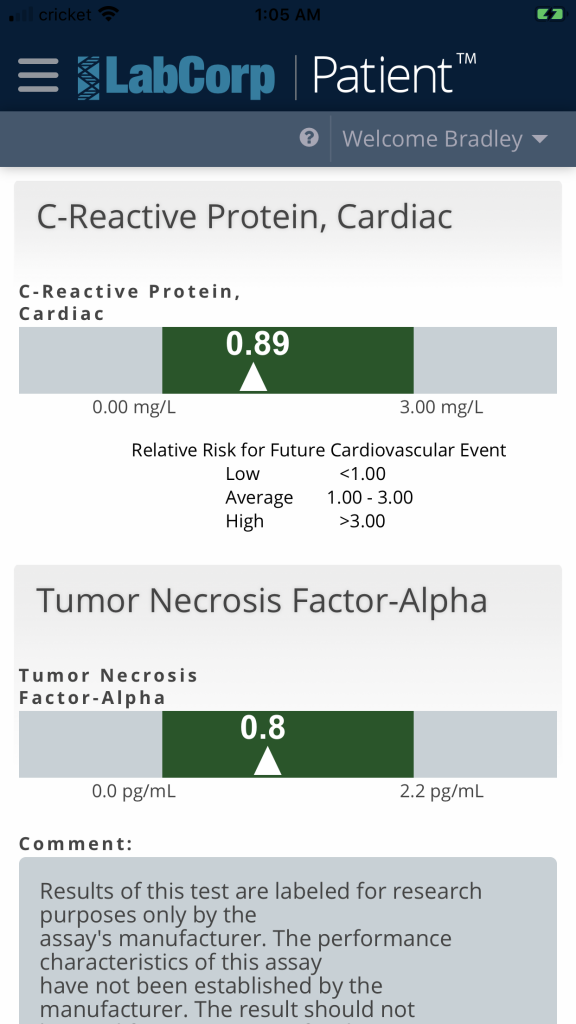
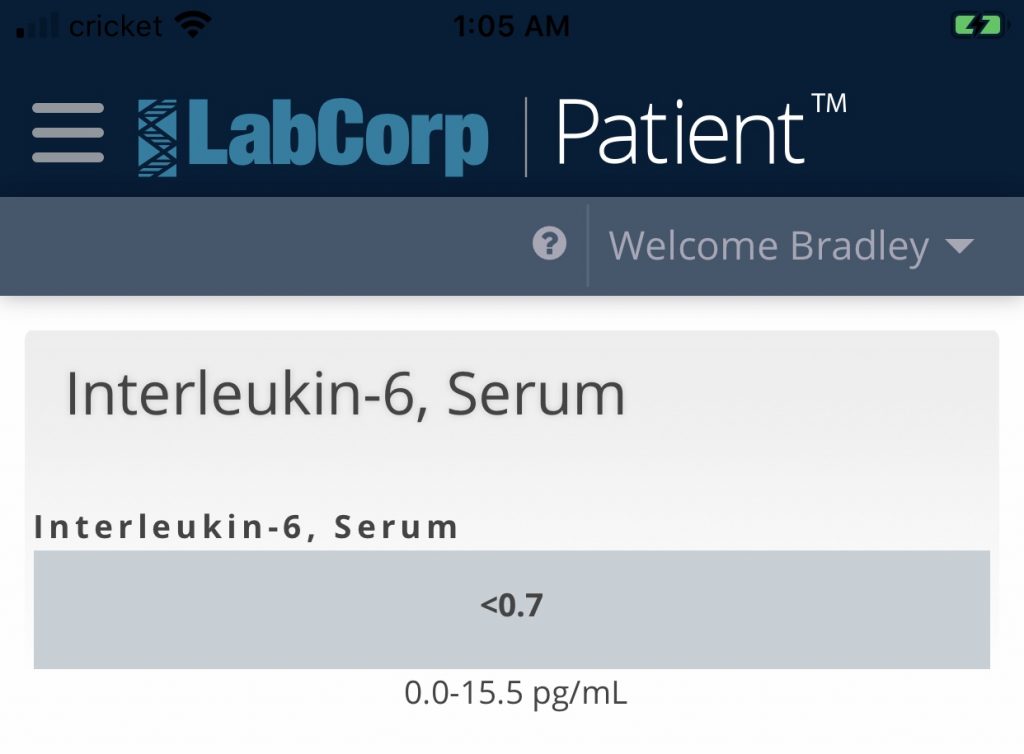
There they are! All three inflammation markers are low. They’re not even average, they’re LOW despite the fact that I’m doing everything “wrong”. I am NOT inflamed although I presumably generate a lot of ROS due to my high saturated fat content and low PUFA content.
How Can This BE?!
I’ll defer to the authors of this study. LA means”linoleic acid”. This is the polyunsaturated (PUFA) Omega-6 fat that I have less than 97% of the population. SFA is saturated fat, which I have more than 99% of the population.
Conclusion
Keep it saturated.

Is there any reason to suspect increased stearic acid consumption might cause an acne breakout?
I don’t THINK so. Chocolate supposedly can cause ACNE, but I’ve never attributed it to the stearic acid content.
For the first time in my life I’m eager to get my blood checked. My inflammation is of the charts, but if I check it again in six months time, maybe that will be resolved! That would be something.
It’s obvious to a lot of people that the things we thought to be true in the field of nutrition and metabolism are in fact not. But with every blogpost, with every dietary experiment it’s becoming more and more surreal. Is *everything* we ever knew or thought we knew just blatantly wrong???
I completely understand the wine drinking. You bloody well need it at this point. What will happen next!
We’re all on the crazy train with you, Brad.
I’d suggest that “everything” we knew wasn’t wrong as such. It was incomplete. We were maybe looking at secondary effects and not putting the real levers.
Those inflammation markers are a thing of beauty though. No doubt.
It is a crazy train, though. Could we not all use that right now?
I just at a stearic acid and butter steak (powdered with SA with pats of butter then to cook). I’m pretty damn full. I’ll be interested to see what the next day brings.
I’m sure not hungry now.
While I’m waiting I’m having some wine. Following the Rx.
9/13/1975?
I’m 9/14/1964!
Ha! Fiona Apple is one year to the day younger than me: 9/13/1976
Apparently it is on the low end of omega-6, but 29% still seems very high, doesn’t it?
Or is the blood cell membrane value very different from adipose tissue? I would have expected your omega 6 in the 3% range as well, so what am I missing?
Yes! Membranes need to be very fluid and so are much higher than adipose.
excellent results. It’s been very interesting following the experiment.
Wow! Very nice
What is your blood pressure and pulse like through all of this? Body temperature would be interesting too especially fasting vs feasting days.
Always Brilliant
Brad, Interesting as always.
What’s your take on nuts in general and peanut butter specifically? Too much LA?
Happy birthday,
Richard
Hi Richard!
If I want peanut butter, I buy the PB2 powdered, fat free peanut butter and add butter to it!
Another excellent post, Brad! Thank you for everything you do.
Can you explain how your Omega-6 still accounts for 29% of the fatty acids in your blood profile given how little PUFA you actually get in your diet?
Is this simply a baseline that results from even the minimal amounts of PUFA you consume? Does this represent residual levels that are still coming down as you shed previously accumulated PUFA in your fat cells? Or is there some other mechanism involved?
One part of it is that membranes prefer unsaturated fats for fluidity, so the fat stored in your fat cells will be much more saturated than your red blood cell membranes.
Hi, I have had elevated CRP. I eat a lot of pork rinds. Do you think they have too much PUFA? Thanks for all you have done, you have really opened my eyes!!
Pork rinds can have quite a bit of PUFA! I’m hoping ultimately to have some low-PUFA ones made over at Firebrand Meats!
Hi Brad
Is there any chancee this can be achieved on a vegetarian diet?
No reason it can’t be! I would try to use cocoa butter and coconut oil as the main fats. Consider supplementing a little palmitoleic acid, which is low in vegetarian fats. The reason for this will become clear if you follow this blog in the upcoming weeks.
Also wondering if i use the butter starch ratio combo at every meal i eat?
I think that really depends on you. Some people alternate between zero carb meals and TCD ratios, for instance. I just ate a bunch of pretzels. All starch! I’m not recommending eating straight pretzels, I’m just saying.
Brad, what do you think of salmon? Is the unsaturated fat content problematic?
I think salmon is good. In fact, the EPA and DHA down-regulate SCD1, which is a huge win. I wouldn’t consume fish oil in bulk, there are other issues with that, nut I’m pro real seafood.
hi, how about liver values? sat fat + Alco was protective for mice, which I would expect in here as well.
rgds JR
Liver enzyme numbers were normal, but I’ve got high triglycerides so I have to work on that…
Love it! One question, though: How physically active are you? I’m trying to get a sense of how much these numbers are affected by exercise.
What is the difference in the steric acid contact between cacao butter and cocoa butter? I’m getting confused and having a hard time finding cocoa butter in local stores.
I think they’re the same thing!
Brad